Can 3D Bioprinting “cure” organ trafficking?
The organ shortage leads to organ trafficking.
The global shortage of organs is alarming, leaving thousands of patients in desperate need of organs for severe injuries or illnesses. Globally, more than half a million people are on the transplant waiting list, and many have not lived long enough to receive the life-saving operation. After more than six decades since the first successful transplant, matching organ donors and recipients is the only legal and ethical way to transplant organs.
The dearth of organs for transplant has produced gruesome makeshift solutions. To accommodate this lingering “deadly” demand, there is a whole “lively” black market trading organs, with an estimated value of 1 billion USD, “preyed” on the underprivileged. An exemplified means is that migrants and refugees are coerced into selling their organs to pay for their passage to Europe. In the interview with a Lebanese human smuggler, Syrian refugees were helpless but had to sell parts of their bodies as a last resort for survival; some sold kidneys, while others sold eyes. The United Nations (UN) has placed a primary focus on combating the trafficking of persons for the purpose of organ removal.
3D bioprinting and potential to deliver UN’s Sustainable Development Goals (SDG).
There is a rising hope that 3D bioprinting can remedy the shortage of organs. This, in turn, could discourage people from purchasing illegal organs and help to put an end to this inhumane activity.
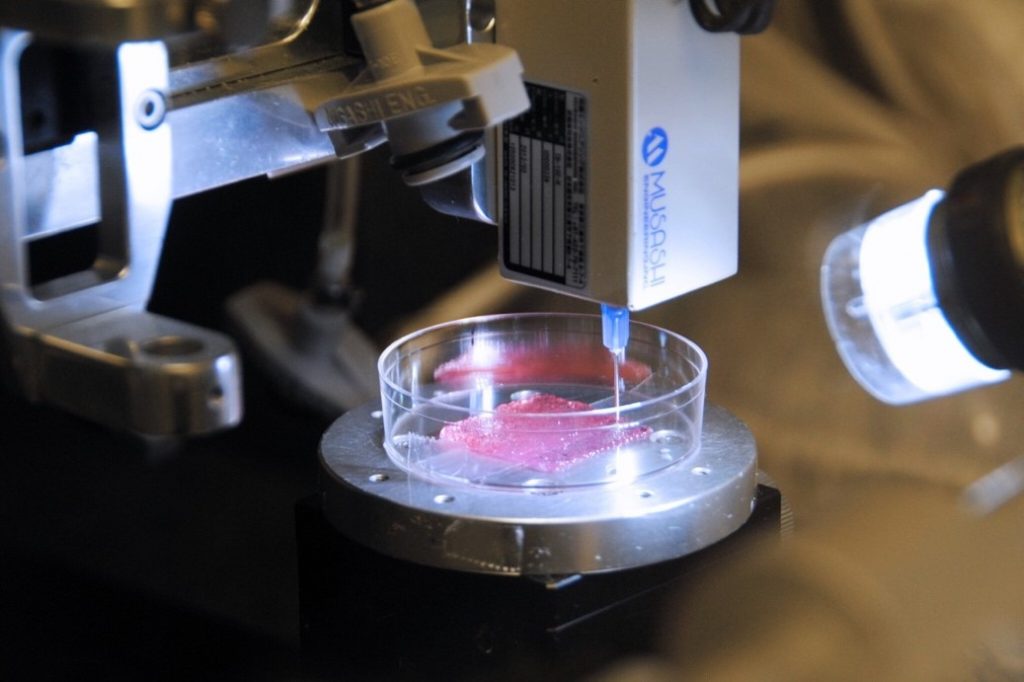
3D bioprinting has emerged as the most promising technology in biotechnology and is expected to have a significant impact on global society in the near future. At its simplest, 3D bioprinting is the same as 3D printing, constructing a 3D object from a digital file, but the material now is from patients’ cells. There have been certain milestones in the application. For instance, Renishaw recreated a cheekbone and eye socket for a road traffic accident victim, enabling reconstructive surgery that would not have been possible otherwise.
More complex structure body parts, such as internal organs (e.g., kidneys, livers, hearts), are under active development. So, it means patients will not have to wait for matching organ donation, with a latent potential of transplant rejection.
Imagine, one day, your kidneys fail and need replacement. Instead of panicking and hopelessly waiting for years for matching organ donation (or illicitly purchasing organs), you only need to wait for acceptable hours to receive new ones just as identical and well-functioned as your “original”.

Advancing SDG 3 and SDG 16 by 3D bioprinting
This technology aligns with SDG 3 – Good Health and Wellbeing by producing body parts that are entirely dependent on donors. if bioprinting can help meet the huge demand for human organs, organs may become more available, and there would be no need to resort to criminal organ purchases. It will eradicate organ trade from the black market – one of the most atrocious transnational crimes, eventually indirectly delivering SDG 16, target 16.2 – ‘End abuse, exploitation, trafficking and all forms of violence’.
The dilemma.
But emerging technologies, which are still in the early stages of development, can paradoxically heighten our sense of uncertainty. The solution to a problem can create many more problems since unforeseen impacts are likely to occur. Although the prospect of this medical technology sounds attractive, it is just the beginning of a big “what if”, including realistic and dystopian risks:
Technological risks:
- What if it is just a fad or here to stay? There is still no guarantee of the success rate of this technology since it remains unproven in clinical practice, with a high chance of irreversible hazards.
- What if the technology is proven to apply safely to humans, but the possibility of erecting a new black market for bioprinters in third countries, where the majority cannot afford the authentic ones? In that case, the quality of fabricated organs made by 3D printers is daunted.
Societal and ethical risks:
- What if organs become commodities, and donors lose the will to donate their organs since the donation is no longer alleged to be noble and meritorious? And it turns out that after a long time, fabricated organs harm human bodies, yet organ donation has run out. So, organ trafficking may escalate and worsen to fulfil the demand influx.
- What if this technology intensifies health inequalities, and only the privileged can access this costly technology while the underprivileged are dying? So, new socioeconomic classes may emerge since only those who can afford them can extend their healthy years.
- What if people can keep renewing themselves like a phone continually updating new versions so that people can be irresponsible with their bodies?
Therefore, the tools of ethical governance and research integrity should be emphasised, especially when humans are involved in experimentation. Because bioprinted products are not apt in the current governance of clinical trials, existing regulations must be reconsidered and possibly redesigned to ensure safety and further development for this promising technology.
Proper governance requirement
Product-based versus Purpose-based approach to governance
In biotechnology, where detrimental uncertainties only reveal after a long time, the governance approach should switch from ‘product-based’ to ‘purpose-based’. The rationale is that product-based governance has been a tremendous concern since it gives more importance to technological risks and ignores risks from other areas (e.g., society or ethics); thus, impacts were later discovered to be harmful to society and environment. In contrast, the purpose-based approach emphasises responsible innovation, including other concerns such as purpose, motivations, and directions.
Responsible research and innovation (RRI)
The purpose-based approach also entails the four dimensions of RRI – anticipation, reflexivity, inclusion, and responsiveness. For instance, socio-literary techniques, which use science fiction to anticipate the future, could be applied to satisfy ‘anticipation’. There are many movies about the future of 3D bioprinting, like Elysium (2013), which depicts 3D bioprinting as used by the rich to create replacement body parts.
Or, more realistic, for ‘inclusion’, bioprinting research in the U.K. involves the process from technological aspects (e.g., Universities, NHS, Medical Research Councils) to social aspects (e.g., Medicines and Healthcare Products Regulatory Agency).
Risk assessment and governance style
“Joint regulation between medical and legal professions is needed to prevent new forces of exploitation”. Hence, the development of 3D bioprinting should simultaneously consider technological risks and embrace ethical, legal and social aspects (ELSA).
This suggestion leads to the appropriate governance style followed. Although in the case of emerging technologies, tentative (learning and experimenting) and definitive (regulative and rule-based) governance should be used together, 3D bioprinting should be developed with ’definitive governance’. Because the application impacts human health, risks are not only at the level of the technology itself but at the societal and ethical levels.
Ultimately, can 3D bioprinting “cure” societal crime?
Technology alone cannot be a panacea for any challenges. To successfully develop an emerging technology, it is important to focus on more than just the technical aspects. It is also true in the case of 3D bioprinting. Technology is undoubtedly a game-changer for the organ deficit crisis. However, 3D bioprinting cannot address the organ shortage crisis, let alone trafficking. The RRI framework and appropriate governance approach should be involved. If 3D bioprinting is successfully and responsibly developed and diffused in society, a foreseen prospect of mitigating organ dearth, eventually organ trafficking, is probable.
About the authors
Ngoc Thuy Trang Tran – A MSc Innovation Management and Entrepreneurship student at the University of Manchester in 2022-23, having obtained a BSc in Marketing in 2019. She is enthusiastic about entrepreneurship in family business and process innovation within existing enterprises, which have the potential to liberate humans from ought-to-be automatic tasks.


0 Comments