
REmote MOnitoring of Rheumatoid Arthritis (REMORA)
The REMORA study will develop, test and evaluate a smartphone app and training video for joints self-assessment to remotely monitor symptoms and disease assessment in people living with rheumatoid arthritis (RA), to support clinical care and research
Patients with RA are asked about changes in their condition at clinic appointments that can be up to several months apart, which means patients may struggle to accurately remember the details of these changes. The app allows patients to record symptoms on a daily basis and log the impact of their RA between clinic appointments.
The specific benefits of using remote monitoring of the symptoms for people living with rheumatoid arthritis included:
- providing the “bigger picture” of rheumatoid arthritis by identifying real-time changes in disease activity and capturing symptoms that would otherwise have been missed
- enabling person-centred consultations allowing doctors and patients to look together at trends of symptoms through time and make shared decisions
- empowering patients to organize and self-manage their own health
- providing novel data for research, allowing the community to understand how symptoms change day-to-day and how patients respond to treatment including how quickly
The first phase of the REMORA study ran from 2015-17 when 20 patients with RA tested the app over a period of three months at Salford Royal Hospital. The second phase is due to go live at Salford in the first half of 2021, supported by the development of a training video to help patients self-assess their tender and swollen joints from home. A funding application is currently under consideration that, if successful, will allow us to expand to include many more sites in Greater Manchester and North West London.
Self-examine tender and swollen joints in rheumatoid arthritis
A training video has been developed solely for the purpose of showing patients how to examine tender and swollen joints at home. It has been designed and developed by patients and clinicians working on the REMORA study at the Centre for Epidemiology Versus Arthritis, at the University of Manchester.
In the video, Rheumatology Nurse Consultant Tricia Cornell and Karen Staniland, who has rheumatoid arthritis and is patient and public involvement lead for the REMORA project at the Centre for Epidemiology Versus Arthritis, show people with rheumatoid arthritis how to self-examine for tender and swollen joints.
Frequently Asked Questions from Patients (FAQs)
Why are tender and swollen joints measured?
Assessing the number of tender and swollen joints is really important to help healthcare professionals calculate your disease activity. This tells them how active your rheumatoid arthritis is, and guides treatment. Examining your own joints can be useful for your own understanding and to enable you to report to your health care professional.
What is DAS28?
The most commonly used score in clinics is the DAS28 score. ‘D. A. S.’ stands for ‘disease activity score’ whilst the 28 relates to the number of joints examined. It is made up of 4 components including a tender joint count, a swollen joint count, a blood test measuring inflammation – CRP or ESR – and the patients’ assessment of their health over the last week. Other disease activity scores such as the CDAI, or clinical disease activity score, do not include blood tests.
Which joints should I examine?
The 28 joints included in disease activity scores are the shoulders, elbows, wrists, knuckles, middle joints on the fingers, and the knees. It’s not that the other joints aren’t important, especially from a patient viewpoint, just that they are not included in the measure.
Why are feet not include in the DAS28 score?
People with arthritis often ask why the DAS28 does not include the feet. Research found that the overall score did not differ between using 28 joints and a greater number of joints, including the feet. This is why the feet are not included in the measure. The 28 joint count has since become the standard measure used to assess disease activity in people with arthritis, and in clinical trials. However, the feet are often affected in rheumatoid arthritis, and it is therefore really important that people with arthritis and their clinicians discuss and assess the feet, to make sure that inflammation, and other problems are addressed. If you have problems with your feet please raise them with your rheumatology team.
What is a swollen joint?
Joints might appear swollen for lots of reasons. In rheumatoid arthritis, healthcare professionals are looking for joint swelling caused by inflamed joint lining. This makes the joints feel soft and squidgy, like a grape. It is really important that only those joints which feel soft and squidgy are counted as swollen. This kind of swelling can last a long time, or can come and go quite quickly.
Joints can be swollen for other reasons apart from joint inflammation. Osteoarthritis is quite often present alongside rheumatoid arthritis. Osteoarthritic joints are very hard and bony, and don’t tend to change quickly. Although it will look swollen and can be tender to touch, this swelling is caused by bone, so will feel hard and not squidgy. These hard bony swellings do not count as a swollen joint.
There are other structures around the joints which might make you think they are swollen, when they are not. Swelling outside the joint can include pockets of fluid called bursitis. Bursitis does not count as a swollen joint.
Some people have rheumatoid nodules which are knobbly swellings attached to the skin. Nodules do not count as swollen joints.
The only type of swelling that counts in rheumatoid arthritis disease activity examinations is boggy swelling that feels like a grape, due to inflammation in the joint. In this picture, the knuckle joints are swollen.
What is a tender joint?
Healthcare professionals use the word tender to describe joints that feel painful, or sore. Joints may be tender and swollen, just swollen, or just tender.
How do I know if the joint is tender or how hard should I press on my joint?
You need to press on the joint either until it hurts, or until your fingernails go white. If your joint is tender to touch you don’t need to press any harder, but you will still need to feel for swelling.
How do I know where to examine?
When examining the joint, you need for feel for the joint line which is where the ends of the two bones meet – this is where you will be able to feel swelling, if there is any. The video goes through each joint and explains where the joint line is and how the patient can find it.
How do you know whether you’re in the right place?
This will become easier with time. Feeling where the bones move will help you determine whether you are in the right place.
Why do I get swollen palms?
Swelling can occur in places other than the joints, including the palms and the back of the hands. This is important to pay attention to, but does not count as swelling in disease activity scores.
I often get swelling in one shoulder or one hand but not the other. Is this normal?
Although rheumatoid arthritis is often described as being symmetrical, it is very common for different sides of the body to be affected differently.
Do nodules stay forever?
Nodules often stay for a long time. Sometimes they respond to medical treatment and may shrink, or go away.
Useful links
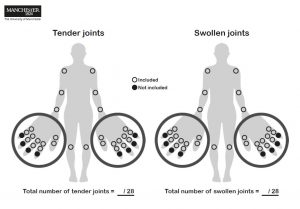 We have developed a rheumatoid arthritis tender and swollen joint count model and table to keep a note of the number of tender and swollen joints during the self-examination. Download the file from here.
We have developed a rheumatoid arthritis tender and swollen joint count model and table to keep a note of the number of tender and swollen joints during the self-examination. Download the file from here.
 Blog post : “How to examine tender and swollen joints: developing a training video for people with rheumatoid arthritis” by Charlotte Sharp, Academic Clinical Lecturer in Rheumatology, who led the development of a video to train people with arthritis to examine for tender and swollen joints.
Blog post : “How to examine tender and swollen joints: developing a training video for people with rheumatoid arthritis” by Charlotte Sharp, Academic Clinical Lecturer in Rheumatology, who led the development of a video to train people with arthritis to examine for tender and swollen joints.
Video development team
The REMORA self-examination video was developed by the following core members, on behalf of the REMORA team
- Tricia Cornell, Nurse Consultant, United Hospital Dorset NHS Foundation Trust)
- Karen Staniland, PPIE Lead for REMORA project
- Dr Claire Smith, REMORA Project Manager
- Ilina Serafimova, Centre Communication Manager
- Prof Will Dixon, Lead for REMORA Project
- Dr Charlotte Sharp, Lead for video


0 Comments